WYPR
March 7, 2019
Rachel Baye
Anne Rowe was diagnosed in 2001 with Von Willebrand disease. It’s a genetic bleeding disorder, meaning her blood doesn’t clot well. The Prince George’s County resident told the Senate Finance Committee Wednesday afternoon that, fortunately, there is a treatment.
“For us to be treated prophylactically only, it could cost us $288,000 annually with no insurance or medications,” she said.
She is currently covered by her parents’ health insurance, she said, and she dreads the day that she’s no longer eligible and may have to choose between her health care and food.
But she said a bill before state lawmakers could help ensure that she can continue to afford her treatment.
The bill, aimed at reducing what Maryland residents pay for prescription drugs, has broad support among elected officials in Annapolis and around the state, but there are questions about whether it is constitutional.
It would create a “Prescription Drug Affordability Board.”
“Say a drug corporation wanted for a new drug to charge $100,000,” Vincent DeMarco, president of the Maryland Citizens’ Health Initiative and the lead advocate for the bill, explained at Wednesday’s committee hearing. “This board would look carefully at what Marylanders could afford, would look carefully at what the drug corporations need, and may conclude, well, in Maryland — you can charge whatever you want around the country, but Marylanders will only pay no more than $20,000.”
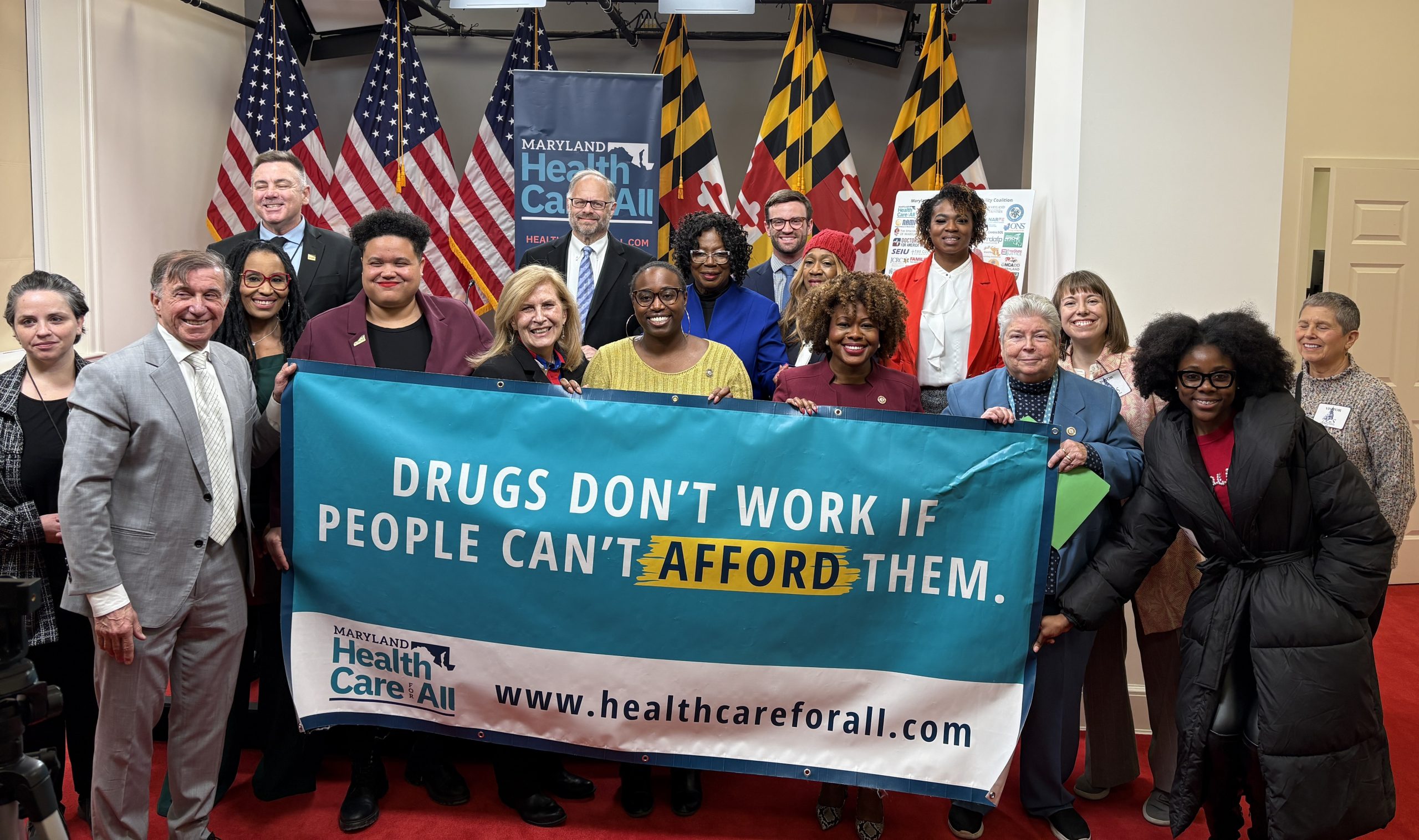
DeMarco has rolled out an extensive campaign with local elected officials to get the bill passed in Annapolis. The Howard, Frederick, Harford and Anne Arundel county executives all testified on Wednesday, and they — along with Baltimore Mayor Catherine Pugh and the county executives of Baltimore, Prince George’s and Montgomery counties — also backed the measure in radio ads.
“I don’t think there’s anybody here that wouldn’t want to vote for this bill,” Senate Finance Committee Chairwoman Delores Kelley assured witnesses at Wednesday’s hearing. “We want to make sure, though, when the bill has passed that it can accomplish — that we’ve structured it in a way to really let it accomplish what you’re hoping can happen.”
In 2017, Maryland passed a law prohibiting the makers of generic drugs from implementing a large price increase without justifying it to the state attorney general. The Association for Accessible Medicines, a trade group, challenged the law and ultimately won the legal battle when the Supreme Court said last month that it would not take up the case.
Kelley asked why this bill would stand up to a legal challenge when that law didn’t.
“What the 4th Circuit said is that it was unconstitutional to have a price control,” DeMarco said. “And what we have in this proposal by Senator [Kathy] Klausmeier and Delegate [Joseline] Pena-Melnyk is not a price control. It’s an upper payment limit.”
DeMarco highlighted a letter from Attorney General Brian Frosh as evidence. In it, Frosh says the legislation is not likely to face the same legal barrier as the 2017 law did. However, he says it could face other legal challenges, including a question on whether the legislation infringes on rights given to drug makers as a result of their drug patents.
But DeMarco compared the proposed board to the system that has set hospital reimbursement rates in the state for decades.
“They don’t set the prices hospitals charge,” he said. “They set what payers pay.”
Leslie Wood, with the trade group Pharmaceutical Research and Manufacturers of America, or PhRMA, said the bill is effectively a price control, despite what DeMarco said, and she said it would be bad news for consumers.
“In countries abroad that have instituted price controls, we have seen severe access limitations for patients in those countries,” she said.
She acknowledged that there is a “drug affordability crisis” but said this bill doesn’t address it. The problem, she said, lies with insurance companies and pharmacy benefit managers, not drug makers. She and other representatives of the pharmaceutical and biotech industries suggested examining the whole prescription drug supply chain.
Last modified: March 7, 2019